Getty Images
I recently had the opportunity to sit down and talk withEric Liederman, M.D., MPH, Director of Medical Informatics forThe Permanente Medical Group,inKaiser Permanente’s Northern California Region, on the topic of telehealth during theCOVID-19pandemic. Kaiser Permanente is a leader in telehealth, andITNis pleased to share Dr. Liederman’s insights with its audience.
According to data from theAmerican Hospital Association(AHA), 76 percent of U.S. hospitals currently connect with patients and consulting practitioners at a distance through the use of video and other technology. According to the AHA, almost every state Medicaid program has some form of coverage fortelehealth服务和私人支付者正在接受许多远程保健服务的覆盖。然而,它的广泛应用仍然存在障碍。我请利德曼博士分享他对远程医疗在大流行期间作用的看法。

Eric Liederman, M.D., MPH
ITN: How did telehealth first come about?
Dr. Liederman:Telehealth encompasses many things — it is a pretty broad term. It refers to care at a distance using virtual technology of any sort. The earliest form of telehealth was via telephone, starting in the 19th century with adoption of phones in people's homes. Physicians were some of the earliest folks installing phone lines so people could summon the doctor, as much care was then delivered through house calls. Getting the doctor to your house before that was a pretty big and slow deal and meant physically sending somebody to go get the doctor. It was the phone call that helped shorten these timeframes. More recently, except for Kaiser Permanente and some other similar organizations around the U.S. there wasn't really a big uptake intelehealthto deliver care. Prior to the COVID pandemic most physicians would only get paid if they saw a patient in person, not over the phone, via video or another virtual modality so few of them did it.
ITN: When the pandemic hit, how did telehealth change?
Dr. Liederman:A big change occurred in March 2020 when theCenters for Medicare and Medicaid Services(CMS) issued a waiver that temporarily allowed reimbursement for video and telephone visits on a fee-for-service basis. In addition, they issued a statement of forbearance of prosecutions around HIPAA violations, surrounding use of non-commercial grade, non-healthcare grade modalities for video care. So, they basically said we'll pay you and you can essentially use any means that you want to do video care, such as using FaceTime or Zoom. Before that, there was very little video care going on and telephone care was generally limited to follow-ups after scheduled visits or test results. With COVID, the use of telephone and video visits grew exponentially because we needed a way to continue to care for our patients in a safe and effective way. Other telehealth modalities have increased in use too — for example we have patients in their homes, using monitoring devices to send weight, blood pressure or oxygen levels to our physicians. It's been challenging for these sorts of things to get off the ground with the fee-for-service reimbursement model. However, an increasing focus on quality outcomes is changing that and so uptake is also increasing.
ITN: How did Kaiser Permanente structure’s help during the pandemic?
Dr. Liederman:At Kaiser Permanente, we have always had an integrated system, with a health plan, medical groups, hospitals and pharmacies all integrated into the delivery system. We have organized ourselves to proactively deliver personalized care efficiently and effectively for our patients and our value-based reimbursement model incentivizes us to deliver high quality care, whether it’s in-person or through telehealth.
Before COVID, Kaiser Permanente was already a leader in the country, I would say even perhaps worldwide, in delivery of video care. In Northern California prior to the pandemic, we were doing thousands of visits per month. Very few other organizations were doing much of anything in this space. When COVID hit, we had to rapidly realign our workflows and we quickly shot up to 40 times the previous volume and now perform hundreds of thousands of video visits per month. We were in a really good position because we already had a very secure and effective platform, but we did rapidly beef up the infrastructure around our existing technology.
ITN: Did anything hamper the telemedicine process once the need became obvious?
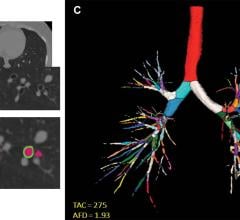
Dr. Liederman:One thing that's hampered telemedicine in general, and certainly teleradiology, is state licensure laws. Most physicians don’t have multiple state licenses to allow for reading across states and various time zones. In some organizations, physicians with a particular state license may move to some other part of the world. Maybe it's Australia, where their day is our night, and because the organization wants to have 24/7 availability for reading x-ray images, as emergency department hospitals never stop. We initiated that approach, within our state boundaries, long before this pandemic, using teleradiology as a service for all of our physicians and hospitals. Many of our radiologists were already working from home using high-powered workstations and multiple high-resolution monitors. So, there was no change whatsoever for us. For other organizations it has likely been more of a scramble.
ITN: How is telehealth being used?
Dr. Liederman:There are many different ways to deliver telehealth; we've talked about two so far: telephone and video visits. With COVID, in order to allow for continuous communication with patients who are in isolation because they have or are suspected to have COVID-19 or some other respiratory condition, we’ve put in place a variety of technologies to allow for video and audio communication. This also saves onpersonal protective equipment(PPE), and it lowers risk to the care team. We also have monitoring technology and are starting to roll out a program to allow certain carefully selected patients who would otherwise be hospitalized, to be sent home and have their hospital care delivered in their own home using remote monitoring and video technology. Surveys have shown that patients really like this. For one, it’s convenient. It also allows patients to be together with loved ones in the comfort of their own home.
ITN: What kind of economic impact has this had, or will it have?
Dr. Liederman:非紧急程序的延迟和取消以及患者就诊的减少对按服务收费的医疗保健组织造成了相当大的打击。我读到过收入下降三分之一到一半甚至更多的报道。尤其是初级保健似乎受到了严重的负面影响,这对这个国家不利。当我们有能力的时候,我们开始改变,至少在某种程度上,因为照顾我们的员工真的很重要,我们不能让这些延误持续太久。Kaiser Permanente在这方面一直很有弹性。
ITN: What does the future look like for telehealth?
Dr. Liederman:目前,我们的一些医生在现场工作,一些在家里工作。我不认为我们会迅速恢复到以前的状态,每个人每天都要通勤去办公室或医院。我认为未来的远程医疗可能会比以前更多;但是,我不知道我们会不会有现在这样多的钱。虽然我们在远程医疗方面做得越来越多,但我们始终保持着提供面对面护理的能力。如果病人需要有人把手放在他们身上,或做一个手术,那么医生就有工具在他或她的指尖使之发生。我希望医疗保健组织和支付者对按人头支付或预付的财务模式有更多的开放,或者从服务收费的角度来看,有某种形式的远程医疗和虚拟医疗支付的延伸。这将使远程保健比大流行病之前得到更大的推广。
ITN:医疗系统从中学到什么?
Dr. Liederman:We are looking atdiagnosis codesand what we call problem reason codes and we're asking which of these tend to end up as doctor office visits, and which don't. The ones that tend to end up at doctor’s offices, we would just book those straight into doctor’s offices. So, we're learning a lot from this.
ITN: What insights do you have that you'd like to share about telehealth and this whole COVID pandemic?
Dr. Liederman:远程医疗方便、安全、有效。我认为第三件事可能是一些人心中的一个问题。有很多文献回溯到一个世纪或更早以前,研究的问题是,仅凭病史就能做出正确诊断的比例是多少,还有通过身体检查,实验室测试,或放射学,或其他方法得到的额外比例是多少。这些研究一致发现,80%以上的情况下,仅根据病史就能做出正确的诊断。这是我们在绝大多数情况下看到的情况。视频访视提供了一定的体检能力,这往往会带来安全、方便、有效的护理,而不需要额外的体检或随访。如果有必要,我们仍然可以通过虚拟护理预约检查。
我给你们举个例子。有一个二、三年级的小女孩得了皮疹,所以她的母亲安排了一次视频探访。那是在上课时间,所以老师只是把病人从教室里拉了几分钟。医生在视频中看到了皮疹,做出了诊断并开出了治疗方案。孩子没有缺课,只是离开教室两三分钟。母亲很高兴,不用花时间在医生的办公室里等待。所以,我们看到很多方便的护理都是通过这种方式提供的。
Also, many people are sheltering in place during this pandemic, wherever they can. I've done telehealth visits with patients who aren’t at home or close to one of our medical offices. They aren’t able to come for a visit, but with telehealth, we can still care for them, no matter where they are.
Telehealth’s Continuing Role in Radiology
While teleradiology and remote reading is not new, its expansion was greatly accelerated in 2020-2021, and continues to grow today, due to the COVID-19 pandemic. Early in the pandemic, hospitals urged their employees to work remotely if possible, and radiologists who wanted to read from home were allowed to do so in large numbers. The past two years has shown many radiologists and clinicians that remote reading from home is indeed possible, and it also can aid the balance between work and family life. Remote reading for radiologists likely will be the new normal, even after the pandemic.
According to a study conducted by researchers atNYU School of Global Public Health,telemedicinevisits accounted for more than 60% of patient care at New York community health centers during the peak of theCOVID-19pandemic in spring 2020.
While video visits have their advantages, telephone visits accounted for a larger proportion of telemedicine care and are critical for providing access and addressing the “digital divide,” according to the study, which waspublished in the Journal of the American Board of Family Medicine.
“Our study suggests that both video and phone visits will continue to shape how healthcare is delivered in a post-pandemic world,” saidJi Eun Chang, assistant professor of public health policy and management at NYU School of Global Public Health and the lead author of the study, in a written statement.
New research published in the October 2021 issue ofJNCCN—Journal of the National Comprehensive Cancer Networkassessed patient satisfaction and preferences for telemedicine with oncology patients, finding 45% of people with cancer preferred telemedicine, while 34% preferred office visits, and 21% had no preference.
The researchers reviewed survey responses from 1,077 radiation oncology patients acrossNCCN Member InstitutionMemorial Sloan Kettering Cancer Center (MSK)’s main campus and six regional locations across New York and New Jersey. In terms of patient satisfaction, most reported either no difference or improvement with telemedicine overall (91%) compared to office visits, with similar results for their confidence in their physician (90%), understanding their treatment plans (88%), and confidence their cancer will be treated appropriately (87%).
“These findings provide some evidence that there is a role for telemedicine beyond the COVID-19 pandemic and that it can be a particularly useful tool for certain patients—especially those who may have challenges coming on-site for an appointment,” said co-lead authorNarek Shaverdian, M.D., MSK Department of Radiation Oncology, in an issued press release. “Giving patients flexibility and options by being able to see them both in-person and through telemedicine can improve access to care.”
Related Telemedicine Coverage:
VIDEO: The New Normal of Home Workstations, Teleradiology and Remote Reading
Telemedicine During COVID-19: Video vs. Phone Visits and the Digital Divide
California Physicians Weigh In On Telemedicine
Just Consider the Possibilities


 August 11, 2022
August 11, 2022